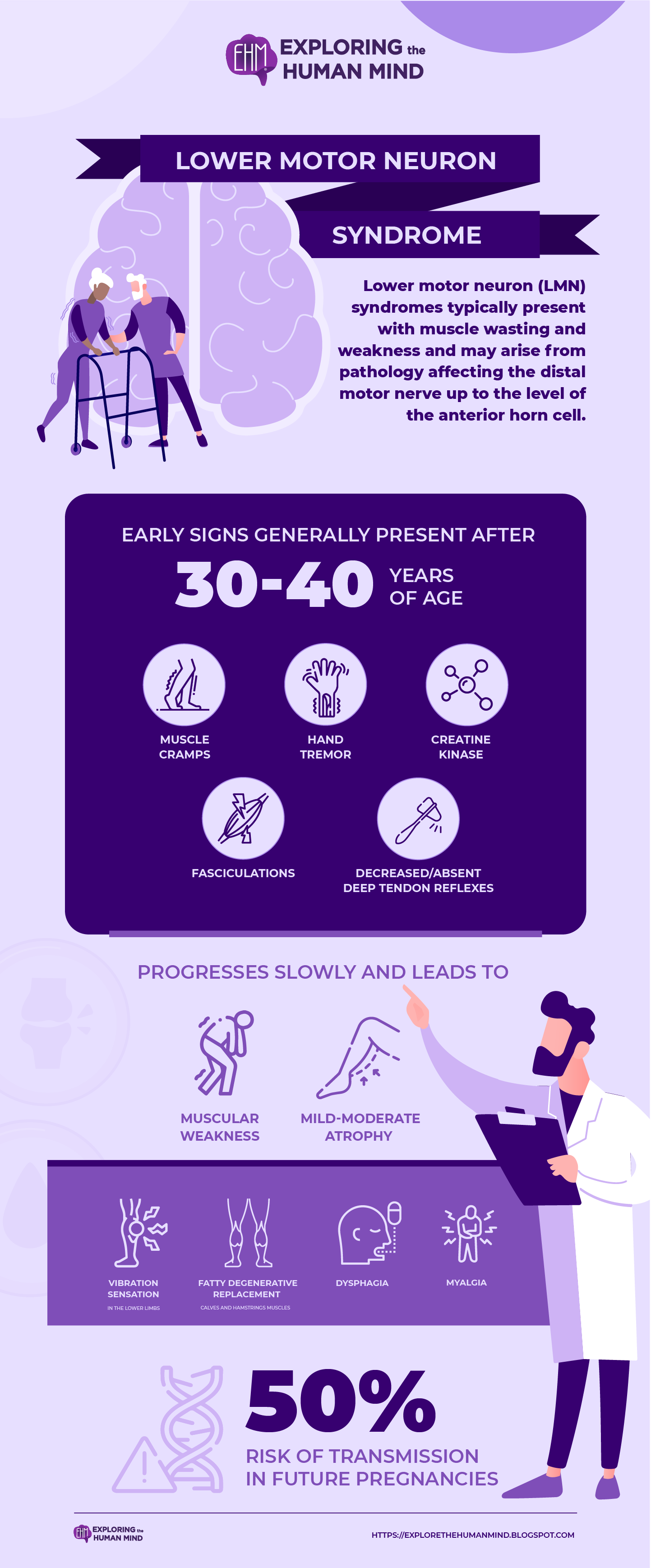
Lower Motor Neuron Syndrome
A rare genetic motor neuron disease characterized by slowly progressive, predominantly proximal muscular weakness and atrophy At the onset, symptoms include muscle cramps, fasciculations, decreased or absent deep tendon reflexes, hand tremor, and elevated serum creatine kinase, is later associated with reduced walking ability and impaired vibration sensation.
Lower motor neuron (LMN) syndromes cause muscle wasting and weakness and can be caused by pathology affecting the distal motor nerve up to the anterior horn cell.
Introduction
Damage to the cell bodies or peripheral axons of lower motor neurons results in paralysis (loss of movement) or paresis (weakness) of the affected muscles. Aside from paralysis and/or paresis, the lower motor neuron syndrome includes a loss of reflexes (areflexia) caused by an interruption of the efferent (motor) limb of the sensory motor reflex arcs. Muscle tone is lost when lower motor neurons are damaged because the tone is dependent on the monosynaptic reflex arc that connects the muscle spindles to the lower motor neurons.
A later effect of denervation and disuse is muscle atrophy in the affected muscles. Fibrillations and fasciculations, which are spontaneous twitches of single-denervated muscle fibers or motor units, may also occur in the muscles involved.
vectors by Freepick; graphic design by Vadot
Genetics
Genetically causes include spinal muscular atrophy, distal hereditary motor neuropathy, and LMN variants of familial motor neuron disease. A number of disease-causing mutations have been discovered as a result of recent genetic advances. Immune-mediated disorders, such as multifocal motor neuropathy and chronic inflammatory demyelinating polyneuropathy, account for a subset of LMN presentations and should be recognized because effective treatments exist. The current review will outline the spectrum of adult-onset LMN syndromes and provide a framework for clinicians evaluating a patient with primarily LMN features.The disease is inherited in an autosomal dominant manner. Affected families should receive genetic counseling, which should inform them of the 50% chance of transmission in future pregnancies.
A pathogenic mutation (p.G66V) in the CHCHD10 gene (22q11.2), which encodes a mitochondrial, coiled-coil-helix-coiled-coil-helix protein of unknown function, causes the disease.
Early symptoms
Early symptoms include muscle cramps, fasciculations, decreased/absent deep tendon reflexes, elevated serum creatine kinase, and hand tremors, and typically appear between the ages of 30 and 40. The disease progresses slowly, causing muscular weakness and mild to moderate atrophy (mostly affecting the proximal lower limbs, with occasional involvement of the distal upper limbs and abdomen). Later in life, patients may develop impaired vibration sensation in the lower limbs, and some may develop mild dysphagia. Other signs and symptoms include myalgia and fatty degenerative replacement, particularly in the calves and hamstrings. Respiratory functions are usually normal, and there are no upper motor neuron signs.
Reference:
Garg, N., Park, S. B., Vucic, S., Con Yiannikas, Spies, J., Howells, J., Huynh, W., José Manuel Matamala, Krishnan, A. V., Pollard, J. D., Cornblath, D. R., Reilly, M. M., & Kiernan, M. C. (2016). Differentiating lower motor neuron syndromes. 88(6), 474–483. https://doi.org/10.1136/jnnp-2016-313526
Purves, D., Augustine, G. J., Fitzpatrick, D., Katz, L. C., LaMantia, A.-S., McNamara, J. O., & S Mark Williams. (2023). The Lower Motor Neuron Syndrome. Nih.gov; Sinauer Associates. https://www.ncbi.nlm.nih.gov/books/NBK11019/
ALL. (2020). Orphanet: Lower motor neuron syndrome with late adult onset. Orpha.net. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=276435



Comments
Post a Comment