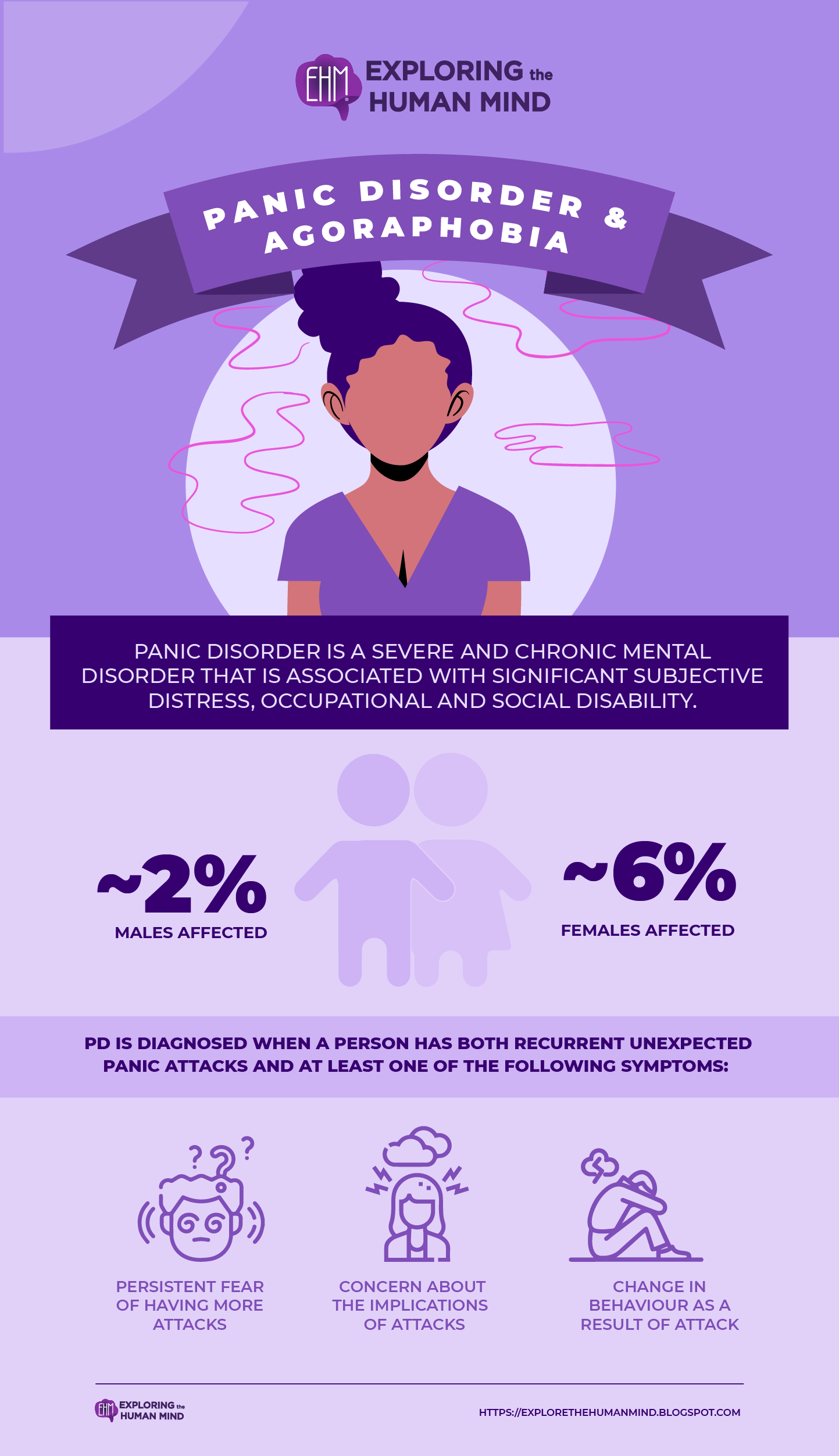
Panic Disorder & Agoraphobia
A panic attack (PA) is the core syndrome (not a codable diagnosis) of panic disorder. Panic attacks are distinguished by their sudden onset, the rapid build-up to a peak, usually within 10-30 minutes, and are accompanied by a sense of impending danger or doom and an urge to flee. According to the DSM IV (APA, 1994), PD is diagnosed when a person has both recurrent unexpected panic attacks and at least one of the following symptoms:
- Persistent fear of having more attacks
- Concern about the implications and consequences of the attacks (heart attack, dying, losing control)
- A significant change in behaviour as a result of the attack.
Furthermore, the diagnosis of PD necessitates a complex set of differential diagnostic considerations because the core feature, panic attacks, can occur as a direct physiological consequence of substance use (i.e., caffeine intoxication) or medical conditions (hyperthyroidism), or in the context of other mental disorders (PTSD, social phobia). PD is frequently associated with agoraphobia (PD with agoraphobia), which is defined as anxiety about being in places or situations from which escape may be difficult or embarrassing, or where help may be unavailable if escape is required.
Agoraphobia is defined by subjective distress and a strong avoidance of such situations. AG frequently co-occurs with PD, but it can also occur on its own (agoraphobia without PD) (APA, 1994). Several epidemiological studies have been conducted on panic disorder (PD) and its associated syndromes and conditions, such as panic attacks (PA) and panic disorder with agoraphobia.
Panic attack rates are consistently higher in females (2.2% for males and 5.6% for females) and at least 2-3 times higher when compared to full-blown panic disorder rates. The 12-month prevalence rates are relatively consistent across age groups and studies.
Agonaphobia rates are difficult to assess because some studies report prevalence rates for agoraphobia in general, whereas others only report rates for agoraphobia without a history of PD. As a result, there appears to be variation in findings. The 12-month total rates range from 0.4 to 3.1%; the median across all studies is 1.3% (range 0.7-2.0), with males accounting for 0.6% and females accounting for 1.5%.
vectors by Freepick; graphic design by Vadot
An abrupt surge of intense fear or intense discomfort that reaches a peak within minutes and during which time four or more of the following symptoms occur:
Palpitations, pounding heart, or accelerated heart rate
Sweating
Trembling or shaking
Sensations of shortness of breath or smothering
Feeling of choking
Chest pain or discomfort
Nausea or abdominal distress
Feeling dizzy, unsteady, lightheaded, or faint
Derealization (feelings of unreality) or depersonalization (being detached from oneself)
Fear of losing control or “going crazy”
Fear of dying
Paresthesias (numbness or tingling sensation)
Chills or heat sensations.
Agoraphobia without a history of Panic Disorder
The individual fears or avoids these situations because of thoughts that escape might be difficult or help might not be available in the event of developing panic-like symptoms or other incapacitating or embarrassing symptoms.
Panic Disorder, with/without Agoraphobia
Persistent concern about additional attacks or their consequences and a significant maladaptive change in behavior related to the attacks.
Reference:
Goodwin, R. D., Faravelli, C., Rosi, S., Cosci, F., Truglia, E., de Graaf, R., & Wittchen, H. U. (2005). The epidemiology of panic disorder and agoraphobia in Europe. European Neuropsychopharmacology, 15(4), 435–443. https://doi.org/10.1016/j.euroneuro.2005.04.006 Panic Disorder and Agoraphobia Criteria Changes from DSM-IV to DSM-5. (2016, June). Table 3.10, Nih.gov; Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t10/





Comments
Post a Comment